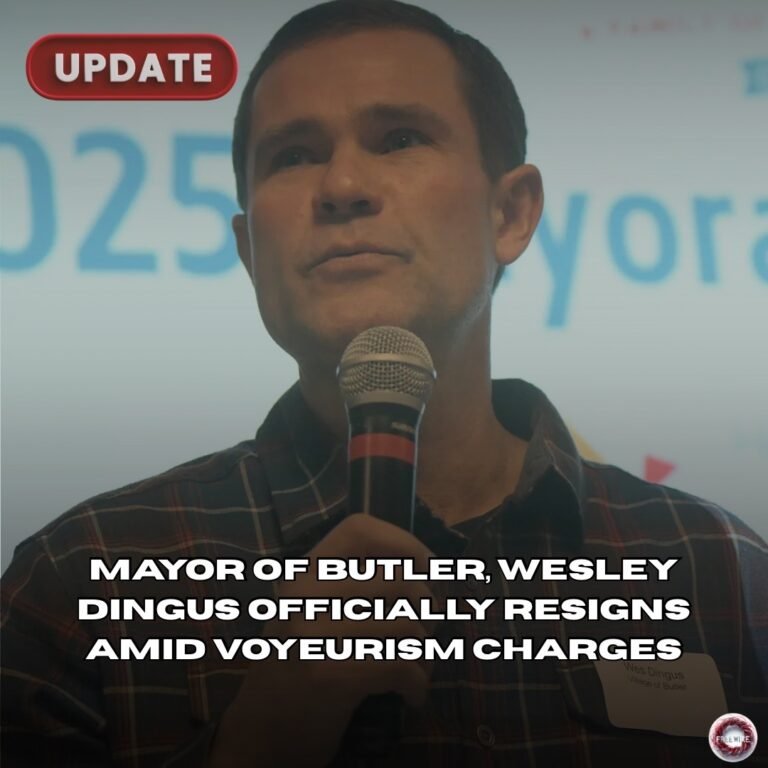
by Logan Andrew | FreeWire Magazine — Your News, Your Voice

When Joshua Goodrich was found with a gunshot wound to the head on October 12th, 2022, his life still flickered. Marion police body-camera video captured officers telling a medic they thought Goodrich was still breathing. Eight minutes later, they saw him move again. But the medic on scene insisted it was “obvious death,” and phoned an emergency-room doctor who advised not to begin resuscitation. Goodrich remained at the scene until an assistant coroner arrived nearly an hour later, realized he was still breathing, and ordered immediate transport. He was finally taken to the hospital, where he lived for about three more hours before dying.
That sequence, now the subject of a federal wrongful-death suit filed by Goodrich’s brother Donald, has rocked Marion County and raised uncomfortable questions about how much discretion paramedics should have in deciding whether someone lives or dies. While the case awaits a jury trial, it also invites comparisons to a troubling pattern of premature death declarations around the country.
What the Marion lawsuit alleges
Rather than disputing the timeline, the lawsuit centers on why medics failed to act. The complaint argues that officers reported signs of life but were overruled, and that the medic’s phone consultation with a physician effectively replaced hands-on assessment. By the time CPR was finally performed and Goodrich transported, precious time had been lost — time his family believes could have made the difference between life and death.
Donald Goodrich believes his brother might have survived if medics had acted promptly. “If it wouldn’t have been for the coroner, they would have just waited there for him to die,” he told WBNS-10TV. The lawsuit names the City of Marion, the EMS team and several police officers. Defendants argue that Joshua showed no signs of life; interrogatory responses quoted by 10TV say the medics “did not perform lifesaving attempts” because he “did not present ‘signs of life.’”
Goodrich’s complaint contends that the responders violated Marion County EMS protocols. Those protocols, as described in court filings, allow paramedics to skip resuscitation if they believe a patient will not survive. Yet Ohio’s statewide guidelines add an important caveat: the state manual lists conditions that allow EMS providers to declare a patient dead—decapitation, decomposition, catastrophic trauma, long-term absence of vital signs—but then warns, “If any doubt exists … resuscitative measures should be instituted immediately and continued until arrival at a hospital or until a physician orders discontinuation.”
As of this month, depositions have been taken and multiple defendants have filed motions for summary judgment. A judge granted Donald Goodrich until 4 September 2025 to respond, and the case is expected to proceed to a jury. Whatever the verdict, the circumstances echo other incidents where medics or remote physicians prematurely ended efforts on people who weren’t yet dead.
Springfield Township: An overdose victim left to die
Earlier this year, two paramedics, a fire chief and an assistant chief in Springfield Township (Lucas County, Ohio) were placed on leave after an overdose call went awry. Responders found a woman unresponsive on a couch and, after contacting a supervising physician, declared her dead. As a coroner’s staff began examining her body, they noticed she was trying to breathe. They administered Narcan and CPR and rushed her to a hospital, where she remained in intensive care. The township administrator said the investigation would determine whether crews followed policy.
The parallels are striking: both incidents involved medics consulting doctors who weren’t on scene; both patients showed signs of life missed by responders; and both resulted in delayed care. The Springfield case didn’t end in death, but it underscores the risk of assuming a motionless or gasping patient is beyond saving.
Other cases across the U.S.
Southfield, Michigan (Timesha Beauchamp)
In 2020, Southfield paramedics attempted to revive 20-year-old Timesha Beauchamp but ultimately called a doctor, who declared her dead without visiting the scene. She was placed in a body bag and sent to a funeral home, where staff unzipped the bag and saw her eyes open and her chest moving. Beauchamp was rushed to a hospital and died two months later. A Michigan appeals court in June 2024 revived her family’s lawsuit, holding that lower courts erred in dismissing the case before discovery. Like the Goodrich case, Beauchamp’s ordeal centers on medics’ reliance on remote medical direction and a failure to recognize residual signs of life.
Clearwater, Florida (Thomas Maxwell)
In February 2023, two Clearwater fire medics responded to 66-year-old Thomas Maxwell, who had suffered cardiac arrest. Finding him “cold to the touch,” they announced he was dead. Yet one minute later, one medic saw Maxwell take a breath—but neither paramedic acted. Body-camera footage from a deputy later showed Maxwell’s jaw moving, contradicting the medics’ report. Another crew eventually transported Maxwell to a hospital; he was discharged a few days later. Clearwater’s fire chief fired both medics, noting that they had access to cardiac monitors and other equipment but chose not to use it.
Houston, Texas (Jacah Jefferson)
The U.S. Supreme Court declined in January 2025 to hear a case involving two Houston paramedics who were sued for pronouncing Jacah Jefferson, a teenager with severe disabilities, dead in 2021. Jefferson’s grandmother called 911 because he was struggling to urinate; the medics, noting no pulse, told her he was dead. A third paramedic arrived, performed CPR and revived Jefferson, but he suffered brain damage. The lawsuit alleged that the failure to administer CPR deprived him of oxygen, yet lower courts held the paramedics immune from liability.
These cases share common threads: remote physicians or medics making death calls without a full assessment, ignoring agonal breathing or minimal movement, and failing to use available monitors. In each, the patient either died or suffered significant harm because resuscitation was delayed.
Why protocols matter
Emergency responders operate under local and state protocols designed to protect patients and providers. Ohio’s guidelines permit paramedics to declare death when injuries are obviously incompatible with life or when vital signs are absent for an extended period. However, the manual’s explicit caution to initiate resuscitation whenever doubt exists suggests that Goodrich’s signs of breathing and movement should have triggered immediate CPR and transport. Experts interviewed by 10TV agree. Emergency physician Dr. Brooks Walsh acknowledged Goodrich’s head wound was devastating but stressed that outcomes can’t be predicted with certainty; he noted Goodrich still had signs of life and said missing information about the phone consultation left many questions. EMS educator Eric Jaeger argued that when a patient is breathing and has a heartbeat, “the right next step would be to assess and resuscitate and transport that patient.”
In Marion’s neighboring counties, this case hits close to home. Bucyrus residents rely on mutual-aid agreements that could bring Marion responders into Crawford County. The prospect of medics misinterpreting agonal breathing or allowing remote doctors to “play God,” as Donald Goodrich put it, is alarming. While paramedics must balance risks—including provider safety and the futility of certain traumas—the Goodrich and Springfield incidents suggest that erring on the side of life may be the safer and more ethical choice.
Looking ahead
As the Goodrich lawsuit moves toward trial, Marion County officials have declined to comment, citing pending litigation. But the public discussion continues. Families of those who died in Southfield, Clearwater and Houston still seek accountability, and Springfield Township is reevaluating its training. Nationally, experts expect more scrutiny of field termination policies and more emphasis on documenting vital signs before pronouncing a patient dead.
For Marion County residents—and their neighbors here in Crawford County—the Goodrich case is not just a legal battle. It’s a call to examine how emergency services handle the most fragile moments of life and death. Was Joshua Goodrich beyond saving? A jury may soon decide. But the cases from Michigan, Florida, Texas and Springfield prove that sometimes, a gasp of air or a slight movement is enough to warrant one more shot at life.